Prediabetes vs. Diabetes: Know the Difference
.jpeg)
Key Takeways
The main difference between prediabetes and diabetes is your glucose level. Prediabetes means glucose levels are higher than normal but not yet high enough for a diabetes diagnosis, which is confirmed when levels are consistently elevated above the normal range.
What to know:
- Prediabetes is also known as impaired fasting glucose (IFG) or impaired glucose tolerance (IGT).
- You can find the specific A1C and fasting glucose levels for diagnosis in the sections below.
- The Nutrisense program provides two glucose biosensors per month and an app to visualize data. Sensors measure glucose in interstitial fluid.
- Lifestyle changes can lower risk in clinical research, often by about 50%. Individual results may vary.
How Prediabetes Differs from Diabetes
Diabetes and prediabetes are two conditions that affect the way the body processes glucose. With the prevalence of these conditions projected to continue to increase over time, it’s important to understand what they are and the difference between them.
That “Prediabetes” Conversation with Your Doctor
You’re at your annual check-up, and the doctor reviews your lab results. Your fasting glucose is 112 mg/dL, and they use the word “prediabetes.” It’s a frustrating moment. You’ve been trying to eat better and stay active, but the numbers on the page don’t seem to reflect your effort.
This diagnosis isn't a final verdict, but a critical fork in the road. It’s the moment you decide to move from guessing what works to understanding exactly how your body responds to your choices.
Let's explore the differences between prediabetes and diabetes, and how to manage and prevent these conditions.
What is Prediabetes?
Prediabetes is a condition in which someone has higher-than-normal glucose levels that are not yet high enough to be diagnosed as diabetes. According to the American Diabetes Association, prediabetes occurs when fasting glucose levels are between 100 and 125 mg/dL.
Prediabetes is becoming more prevalent, and it’s projected that more than 634 million people around the world have prediabetes. At the same time, an estimated 589 million adults are living with diabetes worldwide, and the number is projected to rise to 853 million by 2050.
People with prediabetes are at risk for developing type 2 diabetes, and around five to 10 percent of people with prediabetes become diabetic every year.
Symptoms and Causes of Prediabetes
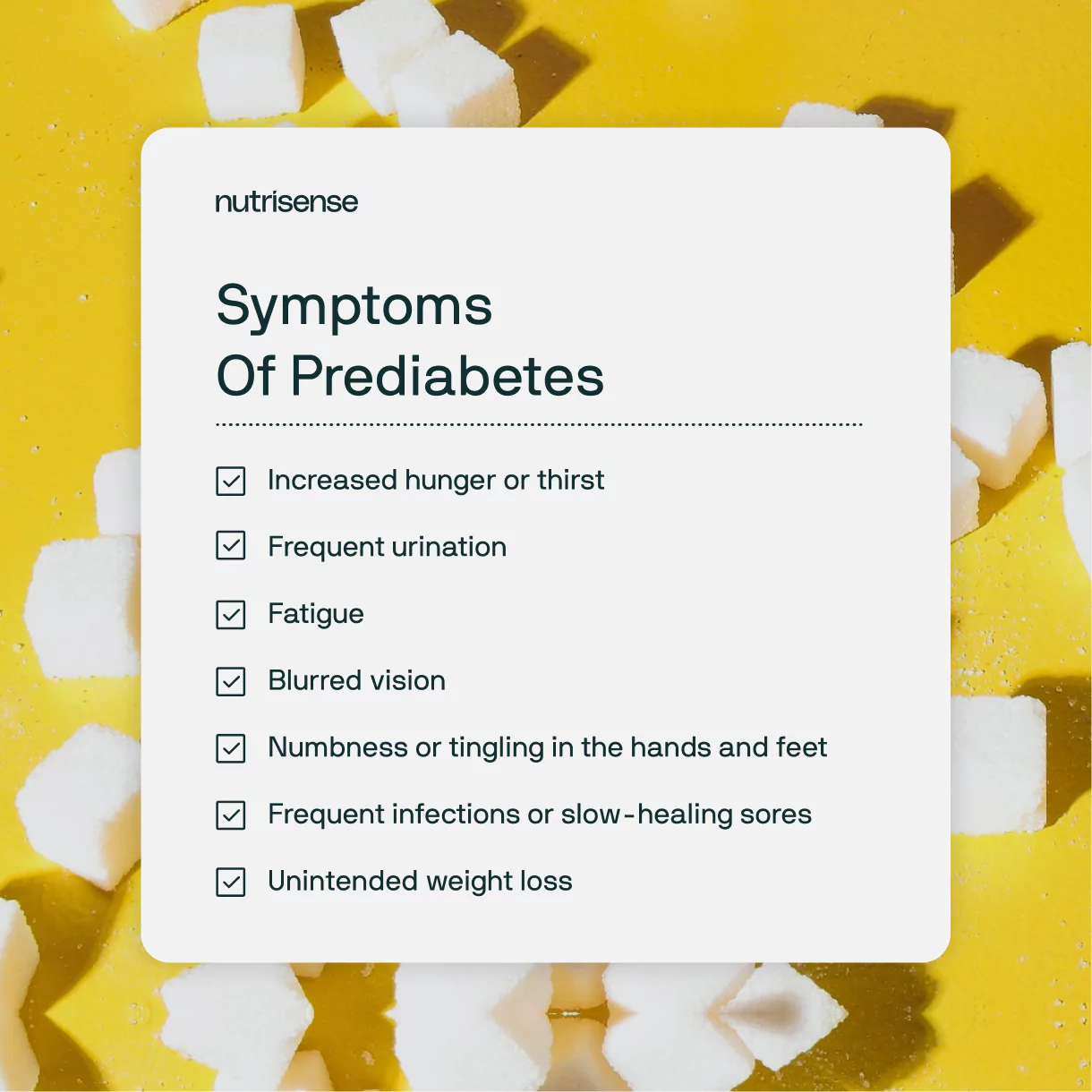
The exact cause of prediabetes is not fully understood, but genetics and family history may influence risk. There are often no obvious symptoms of prediabetes, which is why this condition can only be diagnosed through glucose level testing.
If left untreated, it can progress to type 2 diabetes, which can lead to a range of serious health complications. Here are some of the warning signs that prediabetes has progressed to type 2 diabetes:
- Increased hunger or thirst
- Frequent urination
- Fatigue
- Blurred vision
- Numbness or tingling in the hands and feet
- Frequent infections or slow-healing sores
- Unintended weight loss
The absence of these signs does not mean that you don’t have prediabetes or high glucose, and only a doctor can rule out or diagnose prediabetes or diabetes. If you are concerned about your glucose levels, visit your doctor for further guidance.
What is Diabetes?
Diabetes is a chronic condition in which the body is unable to produce or use insulin properly, leading to elevated glucose levels. There are three main types of diabetes: type 1, type 2, and gestational diabetes.
Type 1 vs. Type 2
Type 1 diabetes is an autoimmune disorder in which the body attacks and destroys insulin-producing cells in the pancreas, causing complications like high glucose and ketoacidosis. People with type 1 diabetes make up about five to 10 percent of all people with diabetes. It often occurs in childhood or adolescence, but it can develop at any time.
Type 2 diabetes, which accounts for the majority of diabetes cases, occurs when the body becomes resistant to insulin and/or doesn't produce enough insulin to meet its needs, causing glucose to build up in the blood. Type 2 diabetes is most common in older adults, but it can develop in childhood as well.
Gestational Diabetes
Gestational diabetes (GDM) is considered a complication of pregnancy and may occur due to changes in glucose tolerance associated with pregnancy. GDM affects approximately 16.5% of pregnancies throughout the world.
Symptoms of Type 1 Diabetes
The symptoms of type 1 diabetes can develop quickly, over a period of a few weeks or months. Some of the most common symptoms of type 1 diabetes include:
- Polydipsia, or increased thirst
- Polyphagia, or increased appetite
- Frequent urination
- Unintended weight loss
- Fatigue
If you notice any of the above symptoms or have risk factors for type 1 diabetes, such as a family history of type 1 diabetes, it's important to get regular check-ups and glucose level testing.
Symptoms of Type 2 Diabetes
The symptoms of type 2 diabetes may develop slowly over time, and some people with the condition may not experience any symptoms at all. But, some of the most common symptoms of type 2 diabetes include:
- Polydipsia, or increased thirst
- Polyphagia, or increased appetite
- Frequent urination
- Unintended weight loss
- Fatigue
- Blurred vision
- Slow-healing sores
- Frequent infections
- Numbness or tingling in the hands and feet
- Areas of dark skin, usually in the armpits or neck
It's important to note that some people with type 2 diabetes may not experience any symptoms or may have mild symptoms that are easily overlooked. As with type 1 diabetes, it's important to get regular check-ups and glucose level testing if you have risk factors for type 2 diabetes or if you notice any of the above symptoms.
Who Is at Risk of Prediabetes and Diabetes?
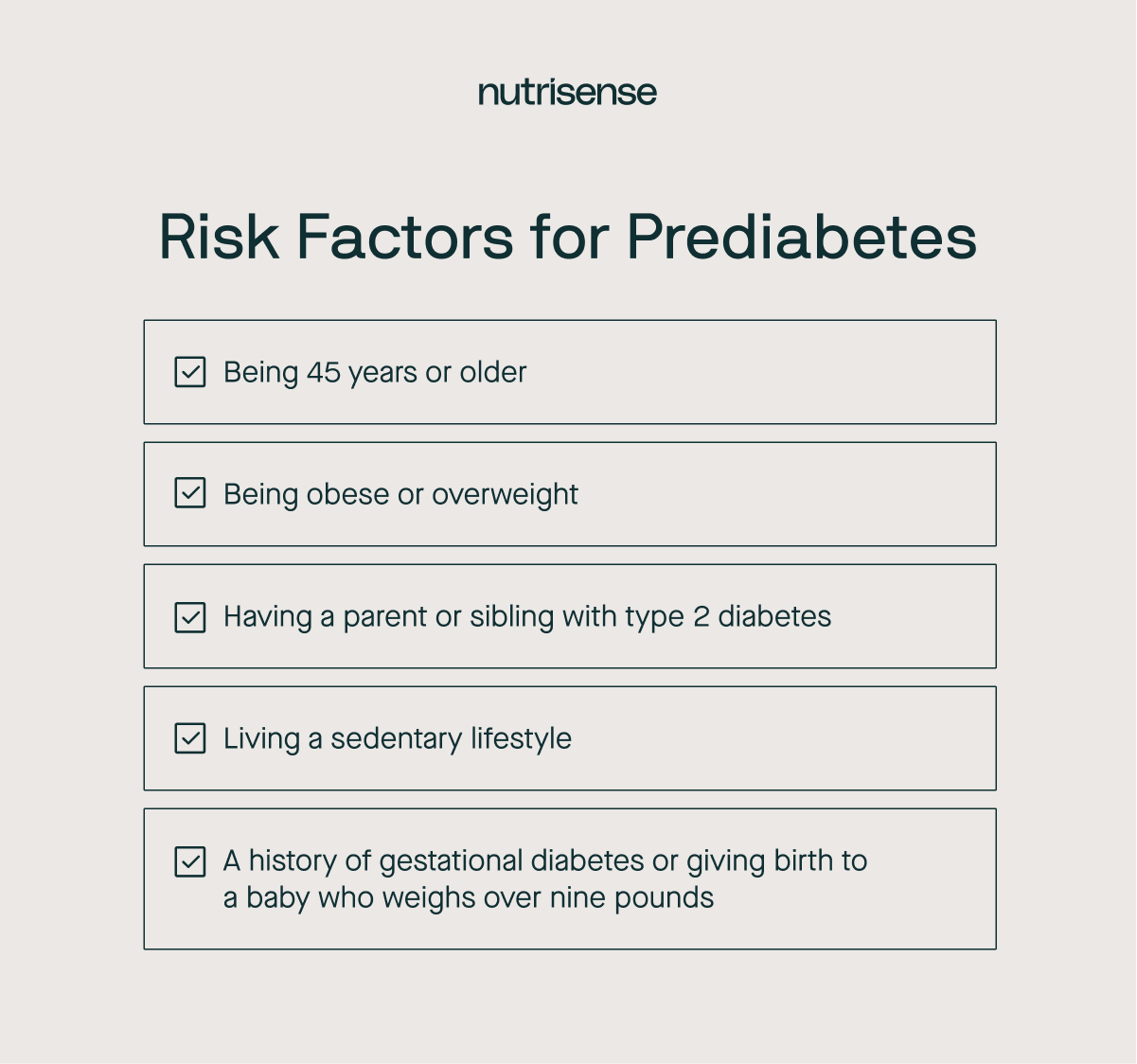
Certain people may be more at risk for developing diabetes or prediabetes.
Prediabetes Risk Factors
Risk factors for prediabetes include:
- Being 45 years or older
- Being obese or overweight
- Having a parent or sibling with type 2 diabetes
- Living a sedentary lifestyle
- A history of gestational diabetes (diabetes during pregnancy) or giving birth to a baby who weighs over nine pounds
Type 1 Risk Factors
Risk factors for type 1 diabetes include:
- Having a parent or sibling with type 1 diabetes
- Age (younger than 14 years old)
Type 2 Risk Factors
Risk factors for developing type 2 diabetes include:
- Being overweight or having a higher waist circumference
- Leading a less-active or sedentary lifestyle
- Having a parent or sibling with type 2 diabetes
- Having prediabetes
- Having polycystic ovary syndrome
Having one or more of these risk factors does not necessarily mean you will develop prediabetes or type 2 diabetes. However, understanding which factors may lead to a higher risk and taking steps to manage them can help reduce the chances of developing these conditions.
What is the Difference Between Prediabetes and Diabetes?

The main difference between prediabetes and diabetes is your glucose levels. Prediabetes occurs when glucose levels are higher than normal - but not yet high enough to be diagnosed as diabetes. Diabetes is diagnosed when glucose levels are consistently elevated above the normal range.
How Are Prediabetes and Diabetes Diagnosed?
Prediabetes and diabetes can be diagnosed through glucose tests, which should be carried out in a health care setting, like a doctor’s office or lab. Here are some of the most common diagnostic blood tests used for prediabetes and diabetes:
When to Get Screened for Prediabetes and Diabetes
Adults should start screening at age 35 and repeat testing at least every three years if results are normal. If you have risk factors or symptoms, your clinician may recommend starting earlier and testing more often. See the screening guidance in the ADA Standards of Care in Diabetes for details on timing and follow-up recommendations.
- If you already have prediabetes, plan on testing yearly.
- Screen sooner if your risk profile changes or you develop symptoms.
Between clinic checks, some people choose to track day-to-day patterns with a continuous monitor to learn how meals, activity, and sleep relate to glucose measured in interstitial fluid. A CGM does not diagnose these conditions. Learn more: What is a CGM?
Hemoglobin A1C Test
The A1C test measures the average glucose level over the past two to three months. A result of 5.7 to 6.4 percent indicates prediabetes, while 6.5 percent or higher indicates diabetes.
Fasting Plasma Glucose Test (FPG)
This test measures the glucose level after an overnight fast. A result of 100-125 mg/dL indicates prediabetes, and 126 mg/dL or higher on two separate occasions indicates diabetes.
Oral Glucose Tolerance Test (OGTT)
This test measures the glucose level after fasting and then again two hours after drinking a glucose solution. A result of 140-199 mg/dL indicates prediabetes, and 200 mg/dL or higher indicates diabetes.
In addition to these tests, a healthcare provider may conduct a physical exam to check for certain symptoms. They may also review the patient's medical history and consider any risk factors for diabetes, such as family history, obesity, and physical inactivity.
Can You Be Prediabetic and Not Get Diabetes?
People with prediabetes have an increased risk of developing type 2 diabetes, but not everyone with prediabetes will go on to develop the disease. Research indicates that there are ways for those with prediabetes to reduce their risk of developing type 2 diabetes, including adopting a healthy diet, aiming for modest weight loss if needed, and regular physical activity.
A large Chinese cohort study tracked adults with prediabetes for roughly 4 years and found that about 1 in 5 returned to normal glucose regulation. People who started with lower A1C and healthier lipid profiles had greater odds of reversal. This shows why early habits matter.
In addition to lifestyle changes, some medications can also be used to prevent or delay the progression of prediabetes to type 2 diabetes. For example, metformin, a commonly prescribed medication for type 2 diabetes, has been shown to be effective in reducing the risk of developing diabetes for those at high risk.
It's important to remember that even if you have prediabetes and never develop diabetes, you may still have an increased risk of heart disease, kidney disease, and nerve damage. Therefore, it's important to take steps to manage your glucose levels and maintain a healthy lifestyle to reduce your overall risk of developing chronic health conditions.
How Are Prediabetes and Diabetes Treated?

If you have been diagnosed with prediabetes, it is important to take steps to reduce your risk of developing diabetes. This may include:
- Lifestyle changes such as eating a healthy diet and engaging in regular physical activity
- Losing weight if you are overweight or obese
- Monitoring glucose levels regularly
- Taking medication if prescribed by your doctor
Lifestyle Changes
Treatment and management of both types of diabetes involves ongoing monitoring of glucose levels and lifestyle changes such as a healthy diet and regular physical activity, to manage glucose levels, prevent complications, and improve overall health.
A healthy diet may include nutritious foods like non-starchy vegetables, lean proteins, healthy fats, and attention to carbohydrate tolerance. Many health professionals also suggest cutting down on saturated fats, added sugars, and refined carbs to help manage glucose.
Regular physical activity is also important for managing glucose, so an exercise routine should be discussed and approved by a doctor. Weight loss for those who are overweight can also be an important part of type 2 diabetes treatment, as it can result in better control of glucose levels.
Medications and Insulin
In addition, medication and/or insulin therapy are often prescribed to help manage glucose levels. People with type 1 diabetes will need regular insulin therapy throughout their life, usually delivered through regular injections or an insulin pump. Some people with type 2 diabetes also require insulin therapy, depending on their level of glucose control.
Foods to Limit If You Are Prediabetic

Here are some foods that you may want to limit or avoid to help manage your glucose levels:
- Sugary foods and drinks: These can cause a rapid increase in glucose levels. This includes candy, soda, juice, sweetened tea, some alcoholic beverages, and other sweet treats.
- Refined grains: Think white bread, white rice, and pasta, which can negatively affect glucose levels. Choose whole grains instead, such as brown rice, quinoa, and steel-cut oats.
- Fried foods and foods high in saturated and trans fats: These foods can contribute to insulin resistance and should be limited. Choose healthy fats, such as those found in nuts, seeds, olive oil, fatty fish, and avocado.
- Processed and packaged foods: These foods can be high in sugar, sodium, and unhealthy fats. Instead, focus on whole, unprocessed foods.
- Processed meats: These meats have been linked to an increased risk of type 2 diabetes and should be limited. Instead, choose lean, unprocessed proteins.
If you're unsure about what to eat or how to manage your diet, consider working with a registered dietitian or a healthcare provider who specializes in diabetes management.
Can Glucose Monitoring Help?
For people concerned with their glucose levels, glucose monitoring can help them learn their patterns. Continuous glucose monitors, or CGMs, use a small sensor under the skin to measure glucose in interstitial fluid 24/7.
Glucose monitoring through a program like the Nutrisense program involves regularly checking your glucose levels to understand how your diet and lifestyle impact your glucose.
Find the right Nutrisense programto turn insight into progress.
Discover the key differences between prediabetes and diabetes in this comprehensive article. Understand the warning signs, risks, and other important information.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. With Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
1:1 Guidance With a Dietitian
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Track Trends and Take Action
With the Nutrisense program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Begin Your Nutrisense Program
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Heather is a Registered and Licensed Dietitian Nutritionist (RDN, LDN), subject matter expert, and technical writer, with a master's degree in nutrition science from Bastyr University. She has a specialty in neuroendocrinology and has been working in the field of nutrition—including nutrition research, education, medical writing, and clinical integrative and functional nutrition—for over 15 years.


.webp)

