9 Tips for Stabilizing Blood Sugar Levels

Key Takeways
Unstable blood sugar levels can be damaging to metabolic health, and if you’ve experienced these imbalances before, you’ll know they don’t feel great either!
Whether you’re looking to improve your overall blood glucose responses or want to adopt a preventive approach to your metabolic health, learning how to stabilize your blood sugar levels is a great first step.
Read on to learn nine tips for stabilizing your blood sugar levels, plus some insightful input from the Nutrisense dietitians on how to detect blood sugar imbalances.
1) Eat a Low Carb Diet

You may have heard the importance of eating a balanced diet. Many automatically interpret this to include the equal amounts of carbohydrates, protein, and fats.
However, the reality is a little more nuanced than that. “Balance” is relative, especially when it comes to your diet and macronutrient breakdown, and not everyone tolerates a high carb, or even a moderate carb, diet.
When you eat a higher carb meal, you may see a higher glucose response since carbohydrates are converted directly into glucose in the blood. If your cells don’t respond to insulin properly (a condition called insulin resistance), then the glucose from your meals isn’t able to be absorbed, leading to chronically high blood sugar levels.
For that reason, low carb foods can be generally recommended to help keep blood glucose levels more stable, or at the very least, prevent a large spike in your blood sugar.
2) Get Daily Exercise
Regular exercise can help reduce high blood sugar and hence stabilize blood sugar levels. According to the American College of Sports Medicine and the American Diabetes Association, all forms of exercise can improve insulin sensitivity and blood sugar control.
However, while any type of exercise is beneficial, different types of workouts will have different effects on your blood sugar.
Steady-state cardio exercises, like jogging or gentle swimming, don’t rely on your body having to produce quick bursts of energy. In these cases, your body will source more of its energy from fat, meaning that your blood sugar will usually stay at the same level or decrease.
Higher-intensity exercises like HIIT, strength training, and sprinting cause your body to release a surge of adrenaline. To ensure that you have enough energy readily available for this, your body releases glucose from your liver, temporarily increasing your blood sugar levels.
Overtime, however, exercise decreases blood sugar in a few different ways:
- Increased glucose can be absorbed without extra insulin (known as exercise stimulated glucose)
- Reduced adipose tissue, or fat, meaning there’s less competition for insulin to get into cells.
- Clearing glycogen stores and increasing glycogen accumulation after exercise.
- Increased metabolic flexibility, which means your body can easily switch between using broken down carbs or fat for fuel.
3) Eat More Fiber-Rich Foods

Fiber helps to regulate blood glucose levels, which can decrease your risk of getting type 2 diabetes.
A meta analysis found that people consuming higher amounts of fiber had significantly lower risk of developing type 2 diabetes than people who eat low amounts of fiber. The two main types of fiber, soluble fiber and insoluble fiber, work together to help stabilize blood sugar levels.
Soluble fiber reduces how much glucose levels increase after a meal (also called postprandial glucose response). This prevents large blood sugar spikes and subsequent crashes. Instead you may feel a steady level of energy throughout your day.
Insoluble fiber reduces insulin resistance. With improved insulin sensitivity, it will be easier for the cells in your body to let the glucose in, leading to more stable and improved levels of blood sugar.
You can include both types of fiber in your diet by consuming things like fruits, vegetables, oats, whole grains, and legumes.
4) Drink Plenty of Water and Stay Hydrated
Hydration is always important, but drinking water can especially help with stabilizing blood sugar in a couple of really important ways.
The first way is straightforward. When you’re drinking water instead of other sugary beverages, you’ll likely be consuming less refined sugar as a result, which is known to spike blood glucose levels.
The second way is that drinking water adds volume to your blood. When you’re dehydrated, there’s less liquid volume in the blood, so your glucose becomes more concentrated (leading to a higher blood sugar reading).
Drinking water reduces glucose concentration, which helps to stabilize blood sugar levels.
5) Eat Less Sugar

Along with consuming less sugary beverages, it can be beneficial to reduce how much sugar you eat.
Refined sugar, as we mentioned previously, is quickly digestible and can lead to a spike in blood sugar. This is especially true if you’re consuming a lot of sugar in a low-fiber meal. However, even sugar variations like honey, which are generally considered to be healthy, can lead to high blood sugar levels.
This may be because honey has a similarly high glycemic index to sugar, which can lead to rapid blood sugar spikes.
Remember, sugar is a type of carbohydrate, so when you’re working to consume fewer carbohydrates, try opting for lower sugar snacks too.
6) Monitor & Reduce Stress Levels
Reducing stress helps to reduce inflammation, helps regulate hunger, and can help to keep your glucose levels stable too. Stress is a reaction in the body that can have many adverse effects on our health, and chronically high stress levels can even encourage insulin resistance and cause glucose spikes.
According to Diabetes UK, stress causes high levels of hormones such as cortisol and adrenaline. These hormones, like inflammatory molecules, will make it harder for your body to respond to insulin properly.
Here are some tips to reduce stress:
- Engage in mindfulness.
- Try breathing exercises
- Try meditation.
- Block off time in your schedule for “me time.”
- Take daily walks.
- Set boundaries.
- Get more sunlight and spend time outdoors.
7) Improve Quality of Sleep & Get 8 Hours of Sleep

Getting adequate sleep is important for your overall health, and it can also help increase insulin sensitivity by reducing stress and mitigating inflammation. Plus, don’t you feel amazing when you’ve had a night of really good sleep?
Not getting enough sleep is also a risk factor for developing insulin resistance. In fact, a study found that even a week’s worth of sleep deprivation results in reduced insulin sensitivity.
So, it may be time to prioritize getting to bed on time and catching those Zs. Here’s a sleep hygiene checklist to get you started in the right direction.
8) Maintain a Healthy Weight & Body Shape
Maintaining a healthy weight and body composition can be very beneficial in stabilizing blood sugar. This is because having a lower body fat percentage means that there are less molecules competing with insulin to get to your cells.
There’s research to suggest that weight loss improves glycemic control in those with type 2 diabetes. Plus, for those with prediabetes, weight loss can decrease the risk of developing type 2 diabetes in the future by improving blood sugar levels.
9) Eat More Protein

Getting adequate protein in your diet can help prevent glucose spikes by slowing down digestion.
The key is to focus on finding the right balance of protein, carbohydrates, and fats for your body. This is where an individualized approach either with a continuous glucose monitor (CGM), dietitian, or both can help you create a diet plan that works for you..
Similarly, a diet high in fat and refined carbohydrates can contribute to insulin resistance, so it can be beneficial to pair your carbohydrates with fiber or protein to improve blood glucose levels.
How Much Protein Do You Need?
When it comes to adequate protein consumption, here’s what the research recommends.
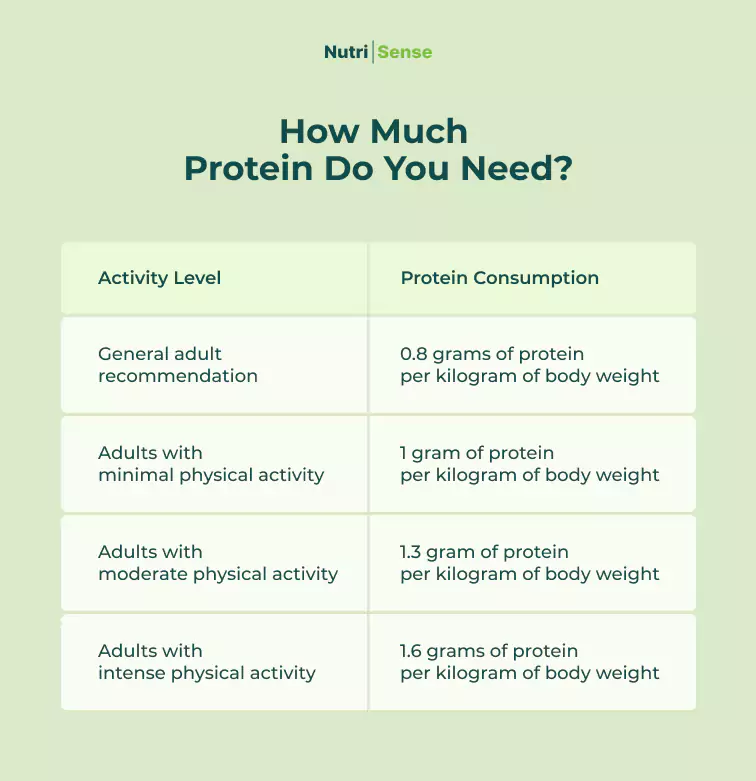
Keep in mind that these recommendations are a starting point, and if you’re looking to build muscle, you may need more protein.
Speak with a dietitian or nutritionist to determine the right range of protein consumption for you based on your weight and activity levels.
Warning Signs Your Blood Sugar Levels Are Out of Control

If you’re unsure whether your blood sugar levels are stable or unstable, let’s discuss some ways to detect poor glycemic control (with expert knowledge from our dietitian team).
Extreme Fatigue
Fatigue is common in those with both type 1 and type 2 diabetes, and can indicate imbalanced blood sugar.
According to Amanda Donahue, MS, RD, CD, fatigue can hit in a variety of ways.
“During exercise, if you're noticing that you're feeling extremely fatigued, or even feel like you completely "bonk" and hit a wall, it could be a sign that your glucose is low and you're not adequately fueled for your workout.
“Alternatively, fatigue can be felt when glucose spikes to higher than normal levels during a workout, which could be increasing inflammation and putting more stress on the body.”
Stephanie Etherington, RDN, CD, CDCES/CDE, explores this further, adding, “One of the classic signs of imbalanced blood sugar is postprandial fatigue.
“This often occurs when people consume a larger portion size of sugary foods or refined carbohydrates, such as flour-based foods, and can be a sign of reactive hypoglycemia. The large influx of easy to digest sugar causes the pancreas to overcompensate by pumping out too much insulin, which plummets the blood sugar lower than when it started. This is often associated with feelings of an energy crash.”
Sugar or Carbohydrate Cravings

Research suggests that intense cravings for high carbohydrate foods can actually indicate low blood sugar levels.
If your meals are irregular or you’re prone to hypoglycemia, it may be a good idea to keep track of your blood glucose levels using a continuous glucose monitor or CGM. CGMs give you 24/7 glucose tracking data making it a helpful tool for those who want a deeper into how their blood sugar levels are imbalanced.
Unusual Weight Gain
Some studies have illustrated that obesity is linked to diabetes or insulin resistance, both of which are marked by high blood sugar levels. The research suggests that those who do not secrete enough insulin to make up for the insulin resistance are at higher risk for becoming obese.
So if you’ve gained weight that cannot be explained by other factors, high blood sugar levels may be something to explore with your doctor or a medical professional.
Trouble Concentrating

According to Diabetes Canada, low blood sugar (or hypoglycemia) can display itself as feeling confused, disoriented, or having trouble concentrating.
If you’ve been experiencing brain fog that cannot be explained by other factors, you may want to check your blood glucose levels.
Excessive Thirst
Excessive thirst can be a sign of high blood sugar. In fact, this condition, otherwise known as polydipsia, is a common symptom in individuals with diabetes.
On the other hand, there may be a link between excessive thirst and low blood sugar stemming from water lost through excessive sweating. Our registered dietitian nutritionist, Katrina Larsen, MS, RDN, LD, CDCES, shares that excessive sweating is a part of a set of symptoms that indicate low blood sugar levels.
According to Katrina, “low blood sugar can come on quickly and it doesn’t feel great! Some signs that your blood glucose is dropping too quickly or too low may include dizziness or feeling light headed, fatigue, increased heart rate, sweating, and nausea.”
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.

Amanda is a Nutrition Manager and Registered Dietitian, with a Masters in Dietetics from Stephen F. Austin State University. Originally from south GA, she got her undergrad degree from Texas Tech University. She worked at a hospital in Fort Worth, TX, for 4 years as a dietitian, counseling those living with HIV.




