Why Glucose Spikes Aren’t Always Bad

Key Takeways
Not all glucose spikes are harmful, as some fluctuation is a normal response to food or even exercise. What matters more than a single event is the overall pattern of your glucose levels. Frequent, large spikes can increase long-term health risks, but brief and occasional spikes might even be beneficial.
Key Takeaways:
- Factors beyond food can cause glucose spikes, including dehydration, stress hormones like cortisol, poor sleep, and even sunburn.
- Learn how to analyze your personal glucose trends to see how your body responds to meals, exercise, and stress.
- Dietitian support through the Nutrisense program may be covered by your insurance.
- A completely flat glucose curve is not the goal, as daily fluctuations are normal and healthy.
When a Spike is a Signal, Not a Problem
As you gain insight into what factors impact your glucose levels throughout the day, you might be wondering more about glucose spikes.
What counts as a glucose spike? And are all glucose spikes bad? How can you know?
In this article, we’ll be exploring these questions and many others related to the science of glucose fluctuations, or glycemic variability (GV).
What is a Glucose Spike and What Causes It?
A glucose spike is a term often used to refer to a rapid increase in glucose levels. But what actually counts as a “spike” is often unclear, as some believe that a glucose spike can range from a slight fluctuation to a far more exaggerated elevation that remains high for several hours.
Common Factors
As glucose levels rise, it prompts the pancreas to release enough insulin to allow the cells to absorb and utilize glucose for energy. Fluctuations in glucose levels occur naturally as a result of the circadian rhythm of hormones involved in the control of glucose homeostasis, as well as factors such as:
- What, when, and how you eat
- Your activity type, frequency, and intensity
- Your sleep quality and quantity
- Your stress levels
- Other health conditions you may have
- Certain medications or supplements
What Counts as a Spike?
Since so many factors can cause glucose to increase, you might wonder how to know when your glucose has spiked in a way that’s worth worrying about.
When it comes to defining a concerning elevation in glucose with a number, things become a little more challenging. Some researchers and health organizations like the American Diabetes Association may consider a potentially harmful glucose spike to involve a glucose reading of anything greater than 140 mg/dL.
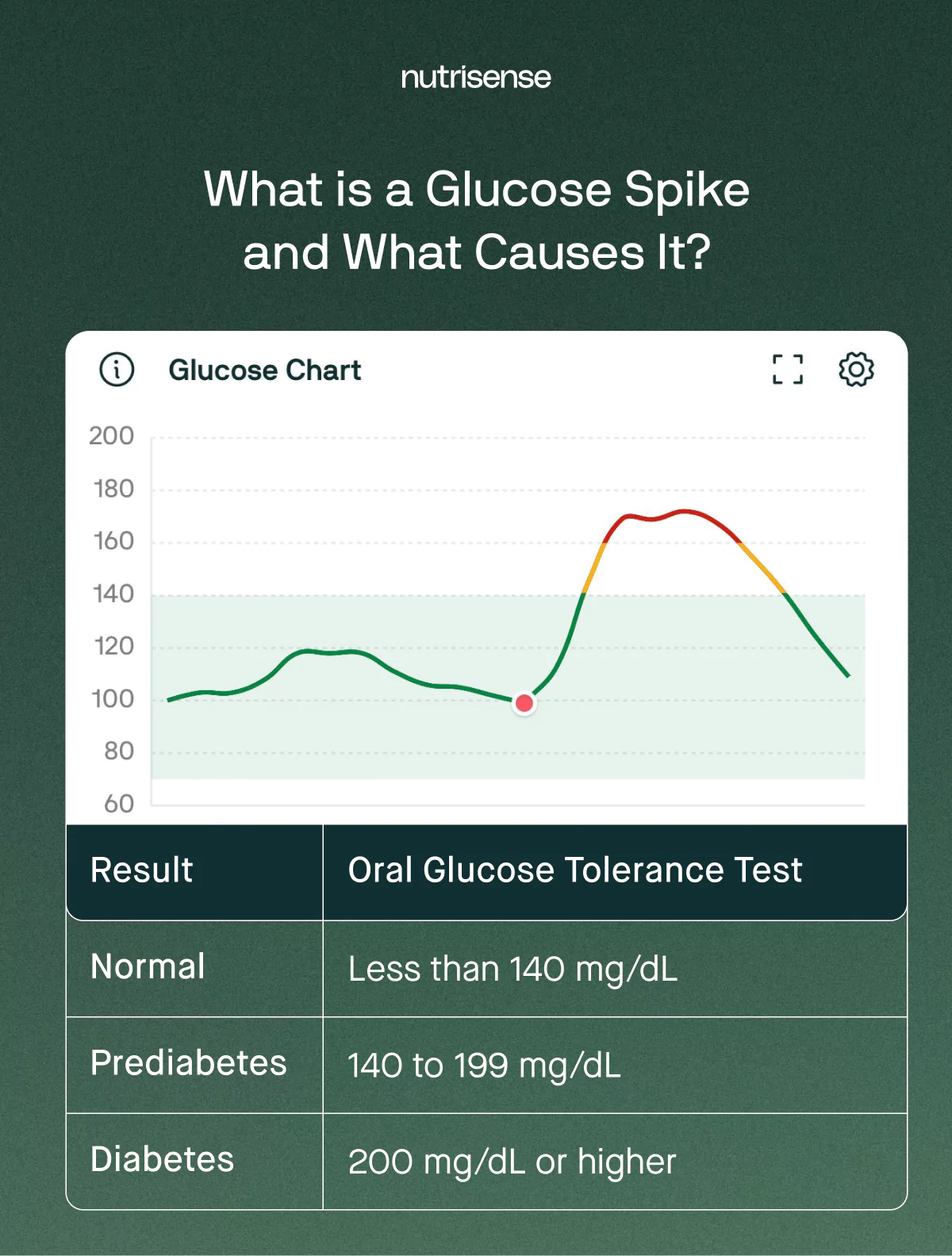
OGTT Ranges
This number comes from the ADA’s diagnostic criteria for diagnosing prediabetes and diabetes, which often uses the oral glucose tolerance test (OGTT). This test measures post-meal glucose response two hours after eating and uses the following diagnostic ranges:
- Normal: Under 140 mg/dL
- Prediabetes: from 140-199 mg/dL
- Diabetes: greater than or equal to 200 mg/dL
This may seem straightforward, but not so fast! Before you think you know all there is to know about glucose spikes, there’s more to consider.
Are Glucose Spikes Normal?

The degree to which your glucose fluctuates is known as glycemic variability (GV). GV, which is best measured with a continuous glucose monitor, which measures glucose in interstitial fluid, gauges how high your glucose rises, but also how low it falls. This can include instances of hyperglycemia and hypoglycemia, or high and low glucose, respectively.
Some degree of variability in glucose is normal and healthy. However, more extreme swings happening more regularly could increase your disease risk over time.
GV and Long Term Health
Glycemic variability is increased in people with diabetes and impaired glucose tolerance and is linked to microvascular and macrovascular complications.
But even in non-diabetics, higher glycemic variability has been associated with an increased risk of cardiovascular disease, Alzheimer’s disease, and cardiovascular death.
In certain studies, researchers even found that dramatic glucose swings may be more damaging than chronic high glucose levels.
Post Meal Spikes and Food Choices
Studies also suggest that diets based on foods that produce lower post-meal glucose responses can improve insulin sensitivity, glucose control, and blood lipid profiles.
At the same time, reducing these post-meal spikes can also reduce the risk of developing conditions like:
- Diabetes
- Heart disease
- Certain cancers
But how low is too low when it comes to glucose? Is lower always better?
The Hidden Dangers of Hypoglycemia
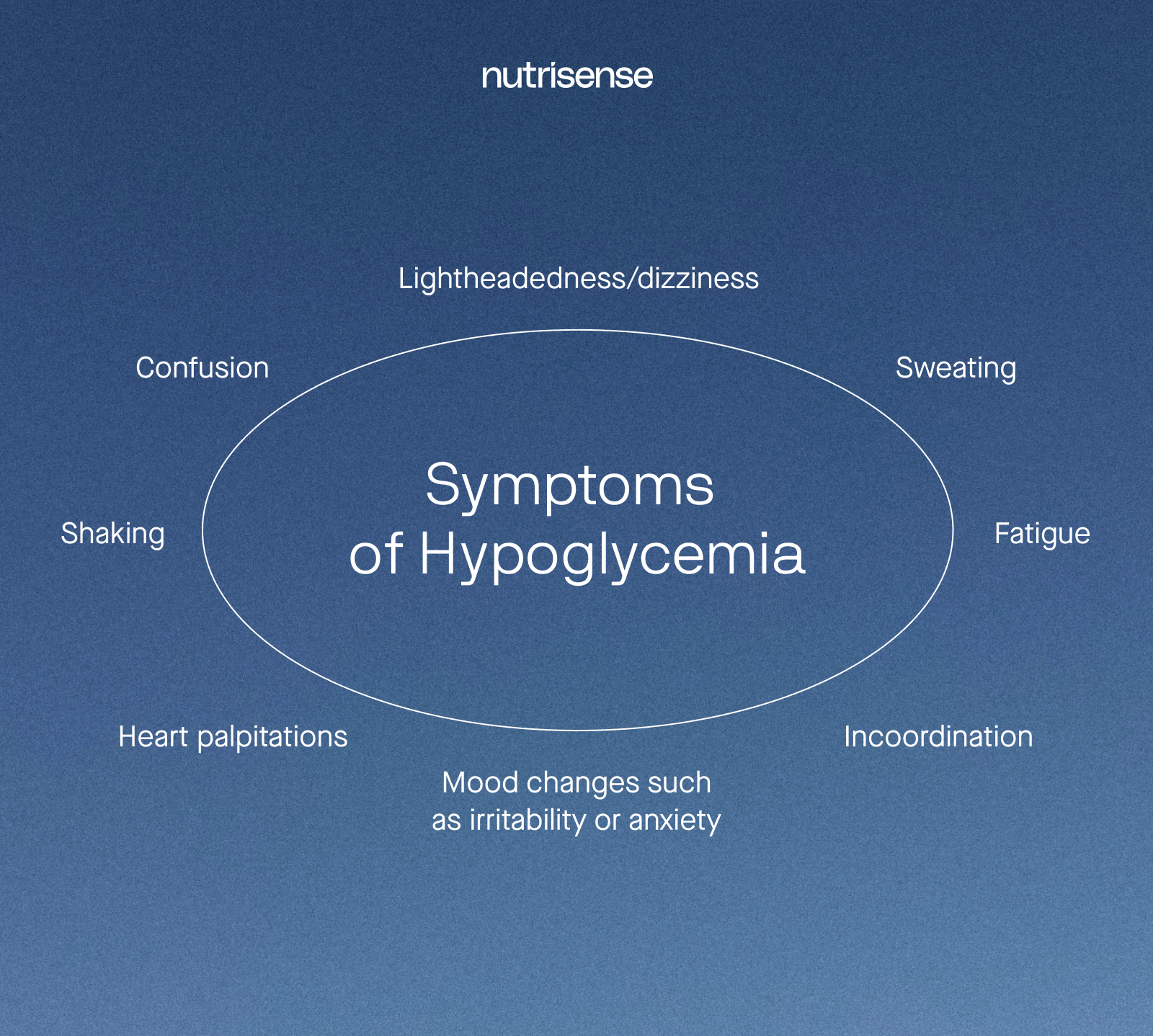
Before we dig more into glucose spikes, it’s important to mention the other side of glycemic variability: low glucose or hypoglycemia. Low glucose is often defined as a plasma glucose concentration below 70 mg/dL with accompanying symptoms.
High GV can come with instances of both hyperglycemia and hypoglycemia, and hyperglycemia is not the only risk for health. Hypoglycemia can be equally damaging in its own right.
There is a significant association between high glycemic variability and the increased incidence of hypoglycemia.
How Lows May Cause Harm
Hypoglycemic events can cause damage by:
- Triggering inflammation by inducing the release of inflammatory cytokines
- Increasing platelet and neutrophil activation
- Increasing a stress response in the body that leads to an increased cardiac burden, among other consequences
Researchers have revealed that high GV, particularly when associated with severe hypoglycemia, could be harmful in people with diabetes and in nondiabetic individuals.
Glycohormesis: Can a Glucose Spike Have Health Benefits?
Glycohormesis is a concept that suggests that being exposed to mild or moderate stressors, such as temporary increases in glucose, might help cells become more capable of dealing with the oxidative stress of higher glucose.
In other words, brief and infrequent glucose spikes might actually be helpful for priming your body’s antioxidant defense mechanisms in ways that could potentially offset the damage of the glucose spikes themselves.
However, as with other examples of hormesis, the dose is everything. Occasional higher glucose spikes are what seem to induce certain cellular protective mechanisms. Chronically high glucose levels and frequent glucose spikes, on the other hand, are more likely to override any potential benefit and lead to higher disease risk over time.
When Should You Worry About Your Glucose Spikes?
Not every single glucose spike above 140 mg/dL may be a cause for alarm, depending on the context. To understand whether or not a glucose spike is really concerning and what you might do about it, you’ll want to consider the following five questions.
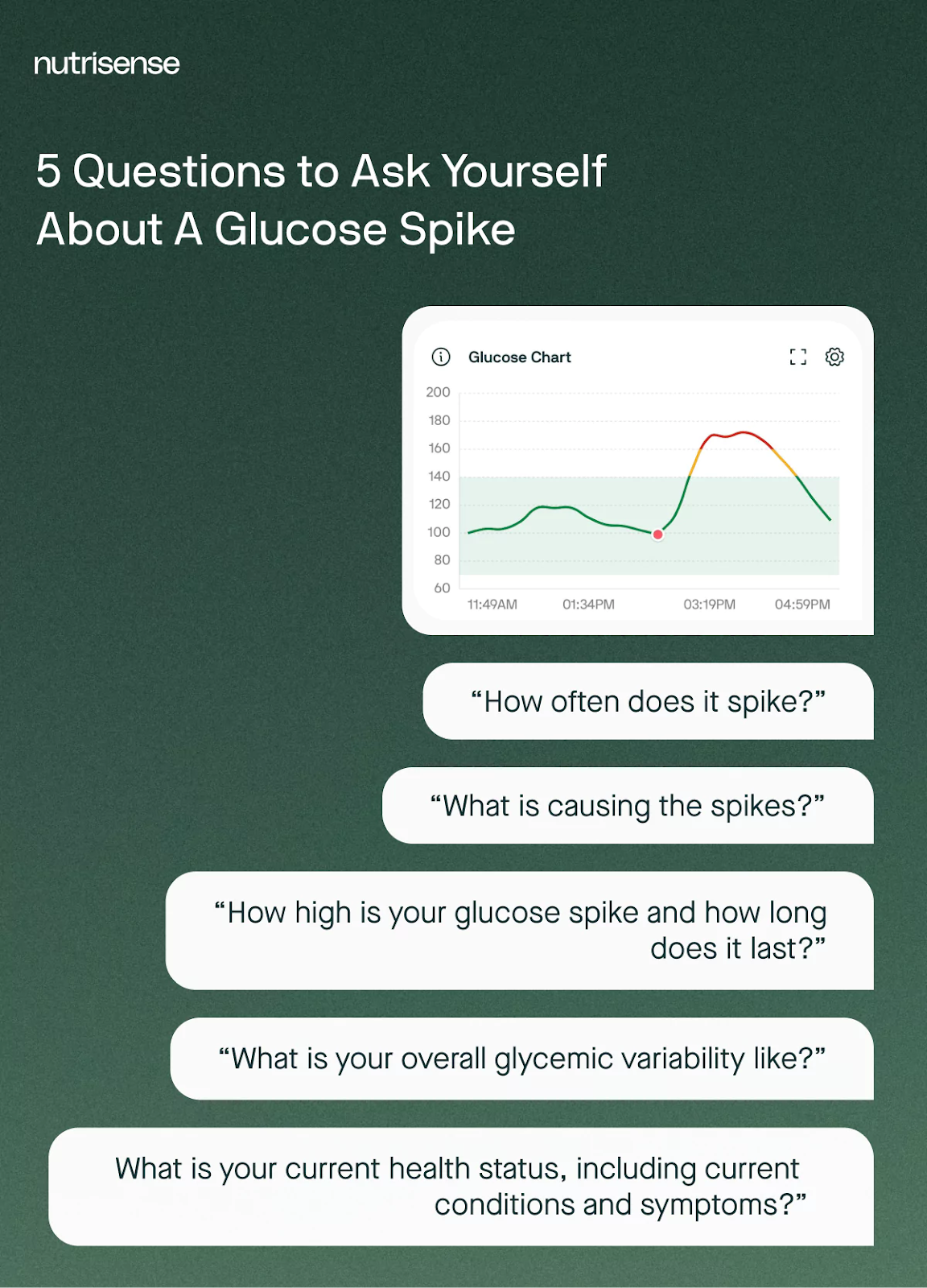
Lab Markers to Consider
Of course, it’s also important to consider lab work from your provider, such as a fasting glucose and insulin level, and other relevant metabolic markers. This added context will paint a much truer and more meaningful picture than simply picking on a single glucose spike in isolation.
For example, a spike of 160 mg/dL may mean something different for someone who is diagnosed with prediabetes and has a higher overall GV paired with frequent high spikes after drinking a sugary drink than someone who is a non-diabetic sports enthusiast experiencing an occasional fleeting spike after running a sprint in the summer heat.
What Causes False Glucose Spikes?
As with any technical device, there are things that can cause inaccurate readings. In the case of continuous glucose monitor (CGM) technology, there are sometimes things that can result in false readings in your glucose data, including false spikes.
These might include:
- Vitamin C, often in higher doses
- Temperature changes, especially more extreme ones, such as sitting in a sauna
- Direct sun exposure to the device
- Some medications, such as Tylenol
- Lying directly on top of the device
What is Healthy Glycemic Variability?

Glycemic variability (GV) is the amount of swing or fluctuation in your glucose levels throughout the day. The definition of glycemic variability is straightforward, but defining what is an ideal or optimal range for GV is a lot more difficult.
No gold standard formula to measure glycemic variability has been identified to date.
Why Defining GV is Hard
Researchers say that defining GV remains a challenge due to the difficulty of measuring it and the lack of consensus regarding the optimal approach for its management.
How GV is Commonly Measured
Standard deviation is often used to assess how much individual glucose values deviate from the average glucose level. A higher standard deviation indicates greater variability in glucose levels or more significant fluctuations over a period of time.
So what standard deviation is considered ideal? A 2023 study used continuous glucose monitors to observe a group of healthy, non-diabetic individuals and found that about 94 percent of glucose sensor values fell between 70-180 mg/dL.
Unfortunately, there is still limited data among non-diabetic populations, and more research is needed to nail down what is optimal.
Other Ways to Measure Glycemic Variability
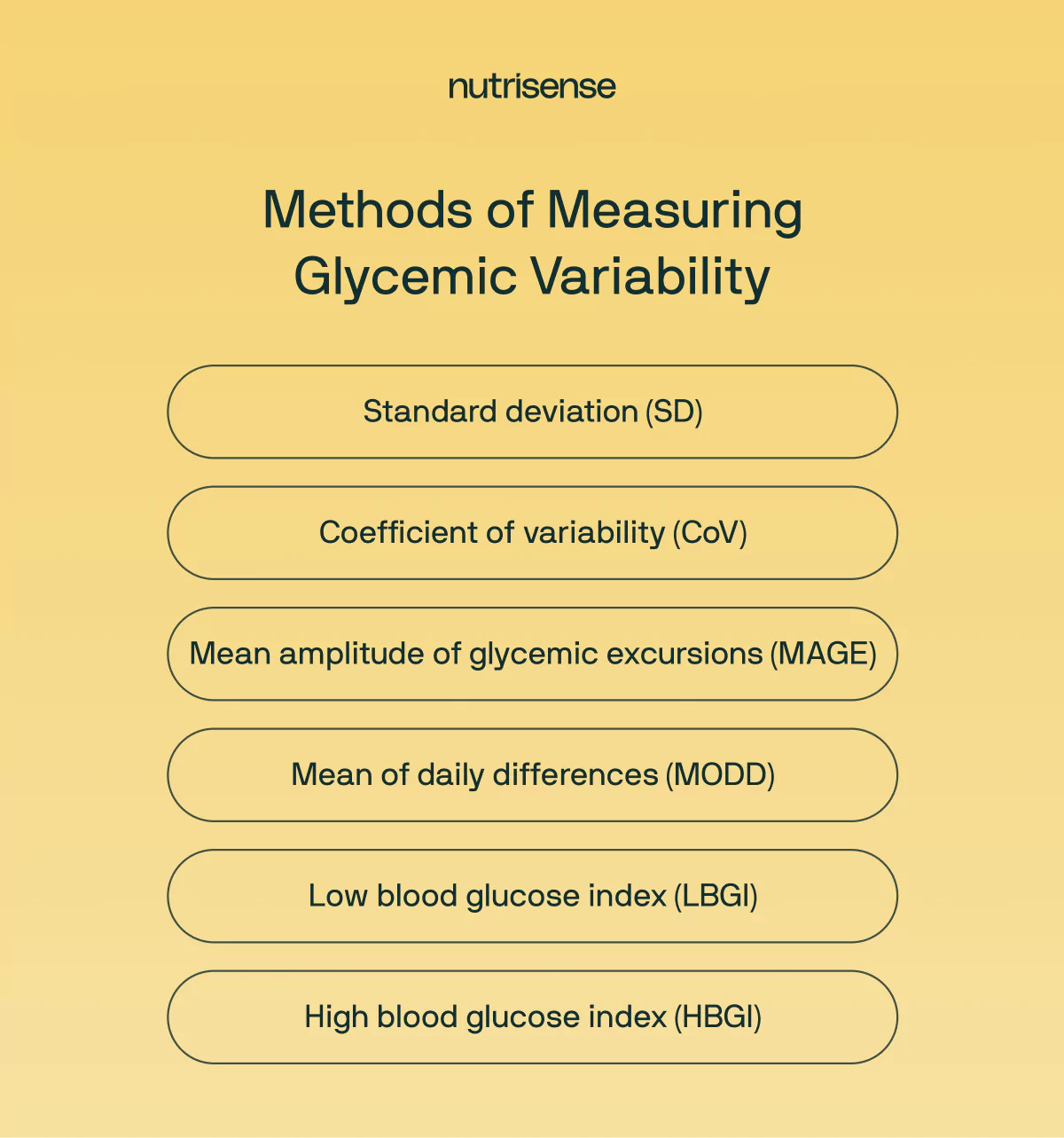
While standard deviation is a useful measure for assessing glucose variability, other metrics such as coefficient of variation (CV) and mean amplitude of glycemic excursion (MAGE) are also often used to provide a comprehensive understanding of glucose fluctuations.
For most cases, SD and CoV may be considered the best variation measures, because they are based on all glucose measurements. However, some believe CoV may be more inclusive and sensitive when compared to SD alone. In those with diabetes, some experts suggest aiming for a CoV of less than 36 percent. For non-diabetics, it’s a lot less clear what is optimal.
For people with diabetes, understanding glucose variability is crucial for optimizing treatment plans and improving overall glycemic control. Continuous glucose monitoring programs like Nutrisense often provide metrics like standard deviation to help you and your healthcare providers assess patterns and make informed adjustments to medication, diet, or lifestyle factors.
Debunking the Myth of Zero Variability
When you first begin monitoring your glucose, you may mistakenly believe it’s all about “flattening” your glucose curve. After all, since “good” glycemic variability is hard to define, should it be assumed that less variability is always better? The short answer is no.
There is no evidence to suggest that anyone should aim for as little variability as possible or that this would be a healthy goal in the first place. Though no research currently outlines the lower limit for variability, it is well-documented that plenty of healthy people thrive with some degree of moderate variability in glucose day-to-day.
Striving for the unrealistic goal of a flat glucose curve is also unlikely to foster a healthy relationship with food, as over-restriction of important nutrients may be required to engineer as little variability as possible.
When a 'Good' Choice Causes a Spike
You finish a tough morning workout, feeling accomplished and energized. But when you check your glucose data, you see a sharp spike, nearly 160 mg/dL. It’s confusing and frustrating. You made a healthy choice, so why does your body seem to be reacting poorly? This is a perfect example of why context is so important. A brief glucose rise from intense exercise is your body releasing stored energy to fuel your muscles.
It's a temporary and functional response, very different from a spike caused by a sugary meal. Understanding these differences helps you move past confusion and build confidence in your choices.
Why Can Exercise Raise Your Glucose?
As you may already know, exercise can sometimes cause a spike in glucose that goes above 140 mg/dL. Is this something to worry about? Nutrisense registered sports dietitian, Kasey Brixius, MS, RDN, CSSD, IFNCP, offers her expertise:
“The mechanism for why the body is dumping out the extra glucose is related to a stress response, and it’s the same as what happens when we are stressed from other sources. Though exercise is often touted as a beneficial hormetic stressor, if you are adding additional stress through improper fueling or poor hydration around your exercise, it can overwhelm the body and lead to even higher spikes.
Some exercise-related spikes can be mitigated from proper hydration as well as proper fueling. We also don't need to push our workouts to that level of intensity in every workout. The body needs time to rest and recover post-stress, and it can't do that if we are going to extremes for every workout.”
Studies with athletes using continuous glucose monitoring (CGM) have consistently shown that athletes have highly individual glucose profiles and often spend a significant amount of time with hypo- and hyperglycemia.
There are many areas of research exploring how glucose regulation affects performance, recovery, and overall health. Authors from the 2023 paper on monitoring glucose in endurance athletes published in the Journal of Sports Medicine state:
“These insights may help athletes tailor their training and nutrition plans to meet their individual needs, ultimately leading to improved performance and better health outcomes.”
So while many questions still remain regarding optimal glucose regulation in athletes, researchers like Dr. Andrew Jagim feel there could be unique value in continuing to track this data over time to get closer to the answers.
Why Do Glucose Trends Matter?
Whether you’re an athlete at the top of your game looking to further optimize performance, someone struggling with a chronic condition, or someone in good health simply wanting to reduce your risk of future disease, understanding glycemic variability can be an important part of your journey.
It’s equally important to ensure you are avoiding the mistake of over-focusing on a single glucose metric, including a single glucose spike, when making decisions about your health or diet.
Instead, tracking trends can provide a comprehensive view of how various factors impact glucose levels. By recognizing these patterns, you and your healthcare provider can make informed adjustments to treatment plans, lifestyle factors, and medication doses.
The Bottom Line On Glucose Spikes

At Nutrisense, we encourage a balanced approach to glucose management that considers overall trends and individual variations. To sum up, here are the key things to keep in mind about glucose spikes:
- Some fluctuation in glucose is normal and healthy, and you should not strive for a flat glucose curve. Always consider a glucose spike within a broader context of patterns over time.
- Glycemic variability (GV) is an equally important metric, but there is very limited research to suggest what is optimal for non-diabetics.
- Chronically high GV may increase risk for cardiovascular disease, diabetes, and other health conditions and complications.
- Continuous glucose monitors (CGMs) are uniquely effective at tracking GV due to the way they are able to capture real-time data over time.
By combining CGM insights with your unique health history, nutrition and activity data, symptoms, and goals, you can help you reach your health potential.
Find the right Nutrisense programto turn insight into progress.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
One-to-one coaching
Sign up to access insurance-covered video calls to work with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
Monitor and measure what matters
With the Nutrisense CGM Program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitor (CGM)s, and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Find your best fit
Ready to take the first step? Start with our quiz to find the right Nutrisense program to help you take control.
Go Beyond Glucose Data with Nutrisense
Your glucose can significantly impact how your body feels and functions. That’s why stable levels are an important factor in supporting overall wellbeing. But viewing glucose isn't enough. With Nutrisense, you’ll be able to learn how to use your body's data to make informed lifestyle choices that support healthy living.
Work With Your Own Dietitian
Sign up to access insurance-covered video calls with a glucose expert: a personal registered dietitian or certified nutritionist who will help tailor your lifestyle and diet to your goals.
From Patterns to Practical Steps
With the Nutrisense program, you can monitor your glucose with health tech like glucose biosensors and continuous glucose monitors (CGMs), and analyze the trends over time with the Nutrisense App. This will help you make the most informed choices about the foods you consume and their impact on your health.
Ready to Take the First Step?
Take our quiz to find the right Nutrisense program to help you take control.

Jordyn has a bachelor’s degree in biology, a graduate degree in Human Nutrition and completed a dietetic internship at the Memphis VA. She's a dietitian at Nutrisense, and has experience working as a clinical dietitian at a VA medical center specializing in oncology and at the Mayo Clinic, working with a wide range of patients ranging from neonates in the NICU to adult ICU.




